Wisdom teeth are the third and final set of molars that most people get in their late teens or early twenties. Sometimes these teeth can be a valuable asset to the mouth when healthy and properly aligned, but more often, they are misaligned and require removal.

When wisdom teeth are misaligned, they may position themselves horizontally, be angled toward or away from the second molars, or be angled inward or outward. Poor alignment of wisdom teeth can crowd or damage adjacent teeth, the jawbone, or nerves.
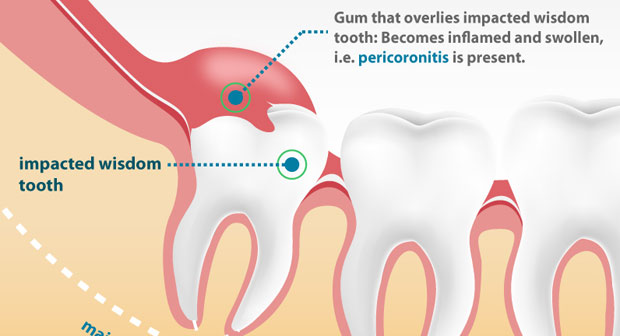
Wisdom teeth also can be impacted — they are enclosed within the soft tissue and/or the jawbone or only partially break through or erupt through the gum. Partial eruption of the wisdom teeth allows an opening for bacteria to enter around the tooth and cause an infection, which results in pain, swelling, jaw stiffness, and general illness. Partially erupted teeth are also more prone to tooth decay and gum diseas,e because their hard-to-reach location and awkward positioning makes brushing and flossing difficult.
How Do I Know if I Have Wisdom Teeth?
Ask your dentist about the positioning of your wisdom teeth. He or she may take an X-ray periodically to evaluate for the presence and alignment of your wisdom teeth. Your dentist may also decide to send you to an oral surgeon for further evaluation.
Your dentist or oral surgeon may recommend that your wisdom teeth be extracted even before problems develop. This is done to avoid a more painful or more complicated extraction that might have to be done a few years later. Removal is easier in young people, when the wisdom teeth roots are not yet fully developed and the bone is less dense. In older people, recovery and healing time tend to be longer.
How Are Wisdom Teeth Removed?
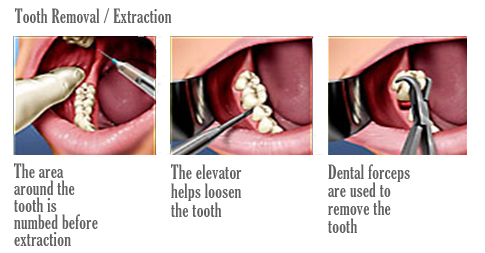
The relative ease at which your dentist or oral surgeon can extract your wisdom teeth depends on their position and stage of development. Your oral health care provider will be able to give you an idea of what to expect during your pre-extraction exam. A wisdom tooth that is fully erupted through the gum can be extracted as easily as any other tooth. However, a wisdom tooth that is underneath the gums and embedded in the jawbone will require an incision into the gums and then removal of the portion of bone that lies over the tooth. Often, for a tooth in this situation, the tooth will be extracted in small sections rather than removed in one piece to minimize the amount of bone that needs to be removed to get the tooth out.
What Happens During Wisdom Teeth Removal?
Before your wisdom teeth are pulled, the teeth and the surrounding tissue will be numbed with a local anesthetic — the same type used to numb a tooth prior to having a cavity filled. In addition to the local anesthetic to numb the pain, you and your dentist or oral surgeon may decide that a sedative is desired to control any anxiety. Sedating medications that could be selected include: nitrous oxide (otherwise known as “laughing gas”), an oral sedative (for example, Valium), or an intravenous sedative (administered via an injection into your veins). If nitrous oxide is given, you will be able to drive yourself home. If any of the other medications is selected, you will need someone to drive you both to and from the appointment.
What Does Recovery Involve After Wisdom Teeth Are Pulled?
After having your wisdom teeth removed, the speed of your recovery depends on the degree of difficulty of the extraction (a simple extraction of a fully erupted tooth versus a tooth impacted into the jawbone). In general, here’s what to expect.
During the first 24 hours
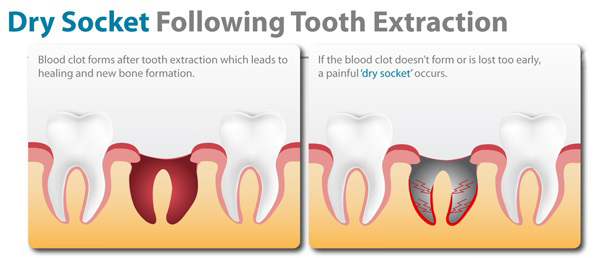
- Bleeding may occur for several hours after tooth extraction. To control it, position a piece of clean moist gauze over the empty tooth socket and bite down firmly. Apply constant pressure for about 45 minutes. A moistened tea bag is an effective alternative. The tannic acid in tea helps healing blood clots to form (blood clots function similarly to scab over an open wound). Repeat this process if a small degree of bleeding continues; if heavy bleeding continues to occur, contact your dentist or oral surgeon. Avoid rinsing or spitting for 24 hours after tooth extraction, avoid “sucking” actions (for example, don’t drink beverages through straws or smoke) and avoid hot liquids (such as coffee or soup). These activities can dislodge the clot, causing a dry socket (see below) to develop.
- Facial swelling in the area where the tooth was extracted typically occurs. To minimize swelling, place a piece of ice, wrapped in a cloth, on that area of your face on a schedule of 10 minutes on, followed by 20 minutes off. Repeat as necessary during this first 24-hour period.
- Pain medications, such as acetaminophen (Tylenol) or ibuprofen (Motrin or Advil), can be taken for minor pain. Your dentist or oral surgeon may prescribe more potent pain relievers, if necessary.
- Antibiotics that may have been prescribed prior to tooth extraction (to treat any active infection around the wisdom tooth to be extracted) should continue to be taken until the full prescription is gone.
- Foods should be restricted to a liquid diet until all the numbness from anesthesia has worn off. Eat soft foods for a few days. Also avoid alcohol if you’re also taking narcotic pain medication.
- Continue to brush your teeth, but avoid the teeth directly neighboring the extracted tooth during the first 24 hours. On day two, resume the gentle brushing of your teeth. Do not use commercial mouth rinses — these can irritate the extraction site.
- Rinse your mouth with warm salt water (1/2 teaspoon of salt in a cup of warm water) after meals and before bed. Do not use commercial mouth rinses.
- Stitches , if used and if not of the self-dissolving type, need to be removed by your oral health care provider in about 1 week. If you do require stitches, ask what type you have been given.
- Watch for signs of dry socket (described below). This condition requires treatment by your oral health care provider.
- Complete healing doesn’t occur for a few weeks to a few months following the extraction. However, usually within the first week or two, enough healing has taken place for use of your mouth to be reasonably comfortable in the area of the extraction. Your dentist will explain what to expect in your specific case.
What Are Potential Complications of Wisdom Tooth Removal?
Two of the more important complications after having your wisdom teeth removed include:
- Dry socket. Dry socket is a common complication that occurs when either a blood clot has failed to form in the extracted tooth socket or else the blood clot that did form has been dislodged. Without clot formation, healing will be delayed. When it happens, dry socket typically occurs 3 or 4 days following the extraction and is accompanied by pain (ranging from “dull” to moderate to severe) and a foul mouth odor. Your dentist or oral surgeon will treat the dry socket by placing medication in the socket.
- Paresthesia. Paresthesia is a rarer complication of wisdom teeth extraction. Wisdom teeth entrapped in the jawbone are often close to nerves. Sometimes these nerves can be bruised or damaged during the tooth removal process. The result is a numbness (called a paresthesia) of the tongue, lip, or chin that can last a few days, weeks, months, or may even be permanent.
You May Interested In: Breast Cancer Is not like the Cancer you see in Movie Anand
